carotid artery disease
- related: Neurology
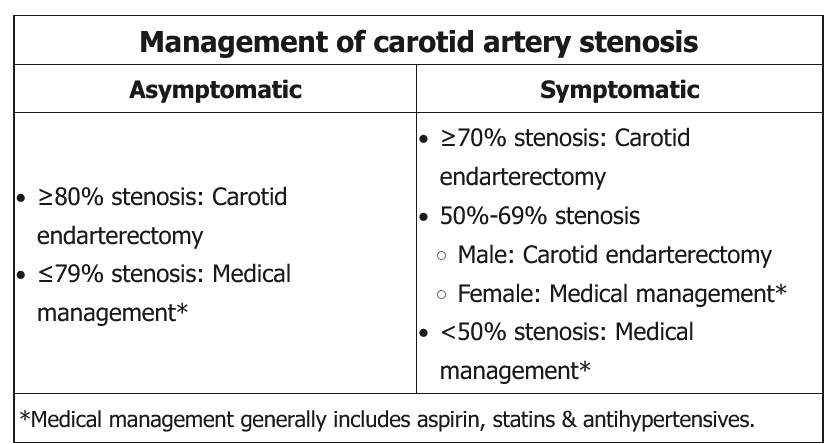
All patients with carotid artery atherosclerosis should receive careful medical management, including smoking cessation, low-dose aspirin, statin therapy, and appropriate control of hypertension and diabetes. In addition, select patients should also be considered for revascularization with carotid endarterectomy (CEA):
- In symptomatic patients (ie, transient ischemic attack or ischemic stroke in the distribution of the affected vessel within the past 6 months) CEA is recommended for high-grade lesions (ie, 70%-99%). Patients unlikely to benefit from CEA include those who are poor surgical candidates due to medical comorbidities, have a life expectancy <5 years, or have had an ipsilateral stroke with persistent disabling neurological deficits. CEA is also not beneficial in patients with complete occlusion of the internal carotid artery.
- In asymptomatic patients, CEA may be considered for high-grade occlusion of the carotid artery, although the exact degree of stenosis at which surgery is indicated remains controversial, and men may benefit more than women. In addition, complete occlusion of the carotid artery in an asymptomatic patient typically indicates adequate collateral blood flow; therefore, CEA is unlikely to provide significant benefit.
This asymptomatic patient has a complete occlusion of the right internal carotid artery and only mild (ie, <50%) plaque in the left internal carotid artery, and so CEA is not indicated (Choice C).
(Choices A and B) Compared with CEA, carotid artery stenting (CAS) is less invasive and may have similar long-term outcomes. However, it is associated with a higher risk for periprocedural stroke and mortality and is generally reserved for patients who may benefit from carotid revascularization but are poor surgical candidates. Carotid bypass surgery is typically considered in situations in which CEA and CAS cannot be performed (eg, redo operations after failed CEA).
This patient developed transient right-sided motor weakness and slurred speech with no evidence of infarction on MRI, suggesting a transient ischemic attack (TIA). Right-sided motor symptoms usually indicate a lesion in the vascular distribution of the left middle cerebral artery, a branch of the left internal carotid artery. MR angiogram of this vessel demonstrated significant stenosis, indicating symptomatic carotid artery disease.
Symptomatic carotid artery disease is diagnosed when a patient with carotid stenosis develops a TIA or nondisabling stroke in the vascular distribution of the diseased vessel. Manifestations typically arise due to either low-flow states (obstructing lesions) or embolic disease.
Patients with symptomatic carotid artery disease who have high-grade (eg, 70%-99%) stenosis and a life expectancy ≥5 years should undergo carotid endarterectomy (CEA) to reduce future risk of stroke. However, the risks of CEA likely outweigh any potential benefits for patients who are poor surgical candidates (eg, multiple medical comorbidities), those with an ipsilateral stroke with persistent disabling neurologic deficits, and those with 100% occlusion of the internal carotid artery.
Surgical management of lower-grade (<70%) lesions is debated among expert panels and depends on sex of the patient and the presence or absence of symptoms. In many cases, patients with such lesions are managed medically only. For all patients with carotid artery disease, medical management includes aspirin, statin, and the control of atherosclerotic risk factors (eg, hypertension, hyperglycemia, smoking).